There is a lot of information about vitamin D importance. I'm going to summarise most important topics and effects and every statement will be linked to scientific evidence. Each image is clickable and linked to scientific sources.
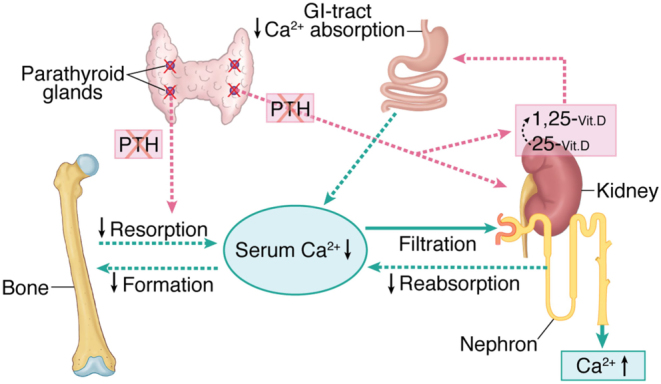
Calcium homeostasis
Calcium (Ca) is required to maintain enough bone density to avoid fractures.
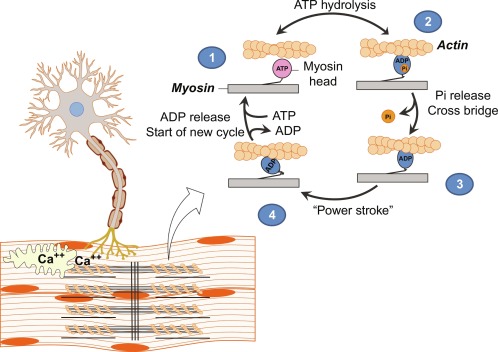
Calcium is required to trigger Ca-dependent muscle contraction.
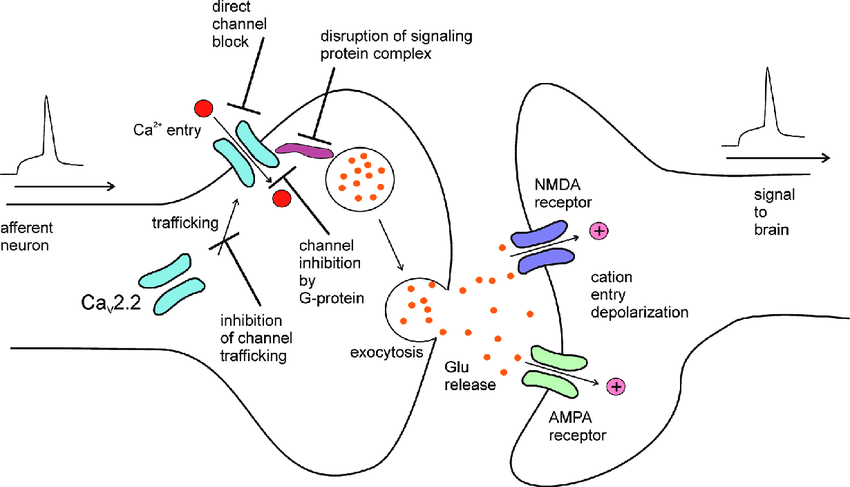
In the nerves electric impulse opens calcium ion channels and calcium influx triggers vesicles to release neuromediator. This happens every time nerve impluse is generated.
Calcium also involved in blood clotting and hormone secretion.
We get calcium only from dietary intake. Active form of vitamin D - 1,25-dihydroxyvitamin D is a major hormone regulator of interstinal calcium absorption. In the absense of vitamin D only 15% of calcium is absorbed. Presence of Vitamin D increase calcium absorption x3-4 times.
We are losing calcium because it's being filtered out by kidneys and Vitamin D promotes calcium re-absorption.
Phosphorus
Phosphorus (P) is involved in a large scale of molecules inside our bodies:
- adenosine triphosphate - main energy molecule
- cellular messengers like G-proteins
- bone mineralization - P and Ca forms bone mineral hydroxyapatite Ca10(PO4)6(OH)2
- cell membrane phopholipids
Absense of Vitamin D reduces phosphorus absorption down to 60%.
Vitamin K
Vitamin K is involved in unique post-translational modification during protein biosynthesis to enable protein function for blood coagulation, bone metabolism, and vascular biology
GLA domain added by Vitamin K to osteocalcin allow it bind calcium ions by chelating them between two carboxylic acid residues. Osteocalcin, matrix Gla protein (MGP), and possibly Gla-rich protein are all inhibitors of soft-tissue calcification and need vitamin K–dependent carboxylation for activity.
When we maintain adequate levels of vitamin D we uptake enough calcium, but Vitamin K deficiency in that state may lead to soft tissue calcification, so adequate levels should be maintained. This why often vitamin D supplements include vitamin K.
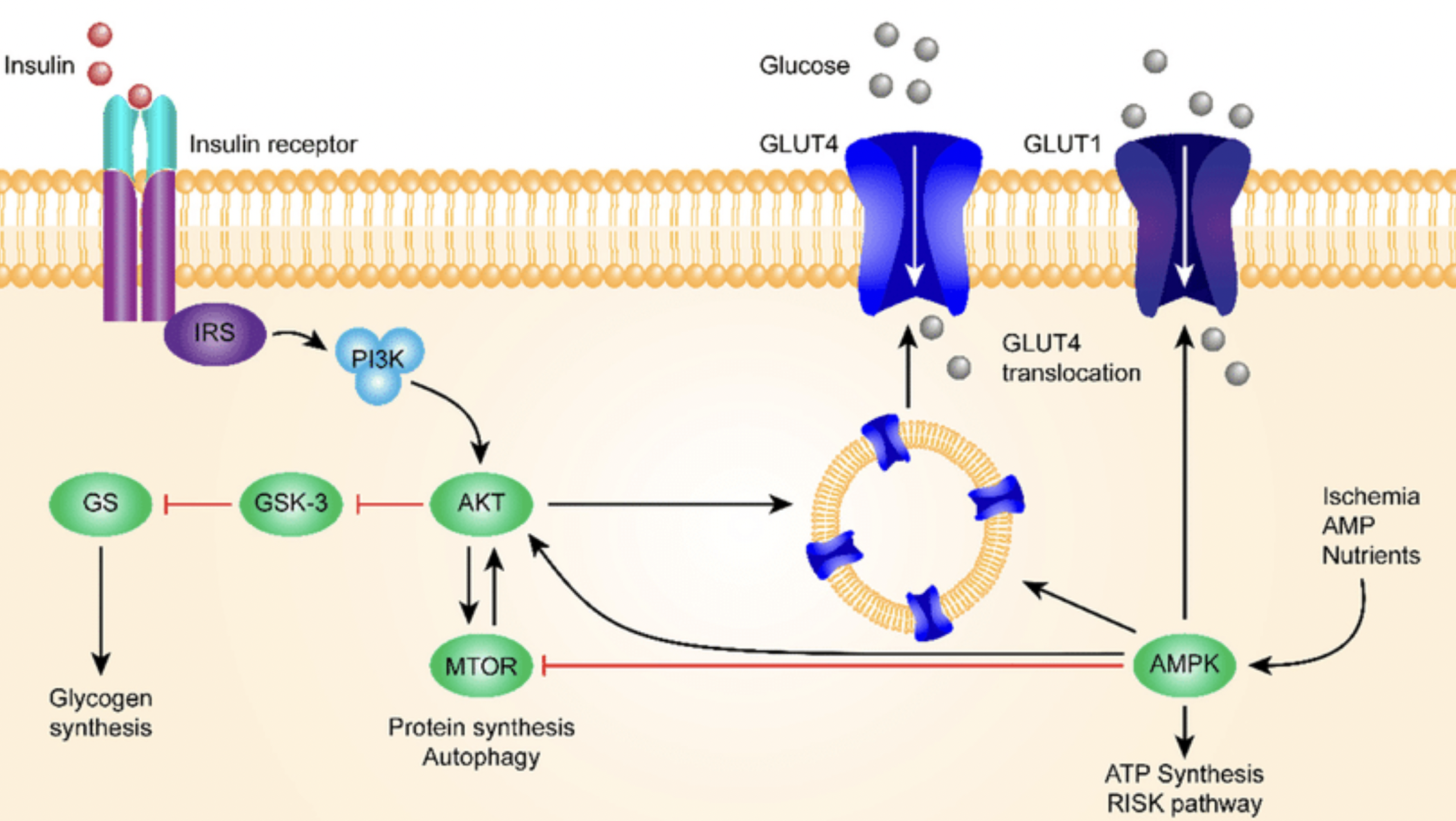
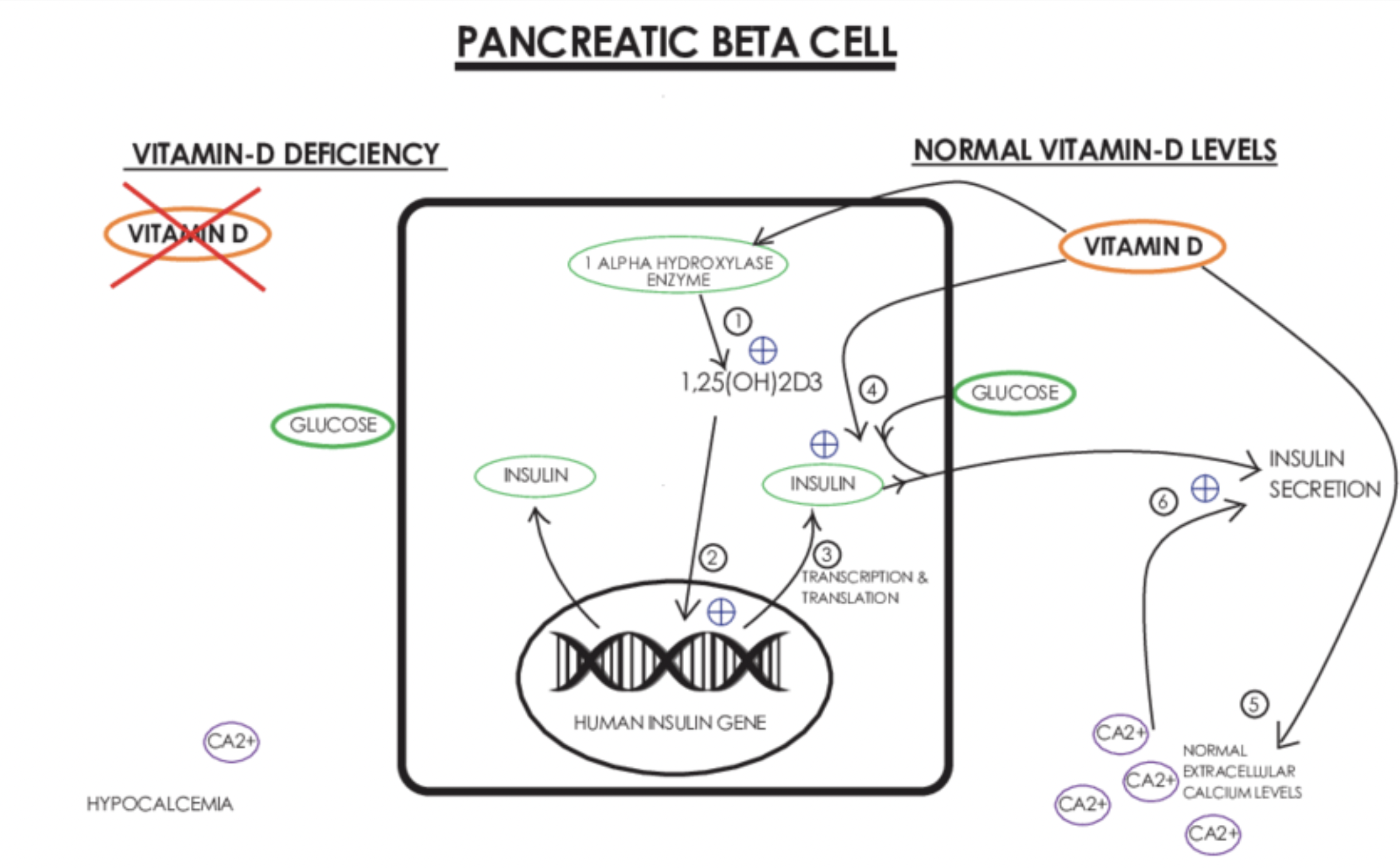
Insulin
Insulin is a main hormone involved in glucose metabolism and anabolic processes.
Insulin is being produced in pancreatic beta cells in response to raise in serum glucose levels. Vitamin D activates insulin receptor gene in nucleus to initiate production.
Vitamin D Receptor
Vitamin D receptor is present inside cell nucleus in the small intestine, colon, T and B lymphocytes, mononuclear cells, brain, and skin. It modulates the function of activated T and B lymphocytes.
There are more than 900 genes regulated by vitamin D.
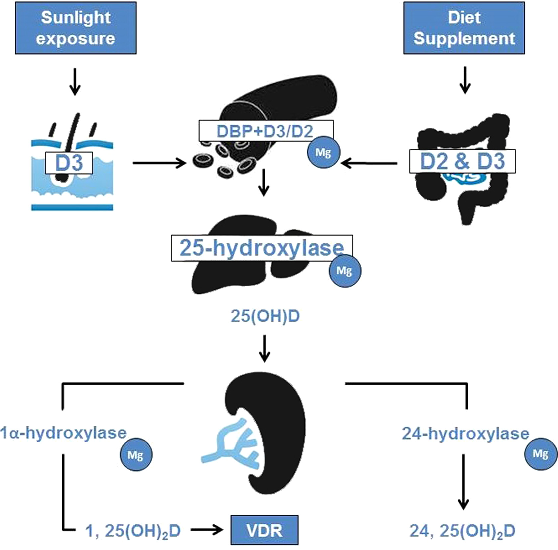
Vitamin D Homeostasis
We get vitamin D from sun exposure and diet / supplements.
Magnesium is required to activate vitamin D through sequence of chemical reactions. Last steps take place in kidneys.
Sun exposure
Skin cells convert 7-dehydrocholesterol to pre-vitamin D3 during UVB radiation exposure and then spontaneously to vitamin D3 by heat.
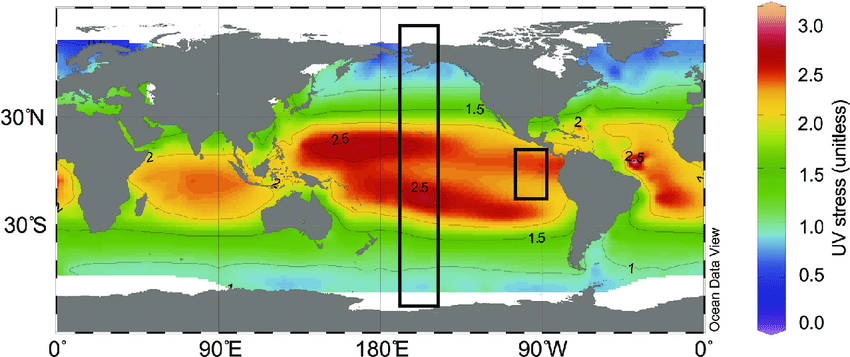
Capacity of skin cells to produce vitamin D is decreased during aging. Melanin in skin cells also prevents conversion 7-dehydrocholesterol to vitamin D. Sun screen protectors greaterly reduce UVB by 95%+ (SPF 8) and 98%+ (SPF 15). During winter and at latitude greater than 37 degree there is decrease in UVB radiation.
There are moderate evidence that adequate levels of sun exposure decrease risks of Type 2 Diabetes and that's might be due vitamin D and insulin regulation.
Diet
There is not too much food with vitamin D - fish, egg yolk and liver. Since vitamin D is fat-soluble and stored in fat tissue and liver - obesity decreases it bioavailability.
Psoriasis
There are data that vitamin D may threat psoriasis, but some novel research puts that into low quality evidence.
Supplementation
Take into account that some DNA polymorphisms decrease vitamin D absorption. Before starting any supplementation serum vitamin D must be measured.
There are some controversial data on optimal range for vitamin D. There are calls to increase normal range to 40-56 ng/ml based on meta-analysis of studies from 1966 to 2013 which shows decreased all cause mortality (ACM).
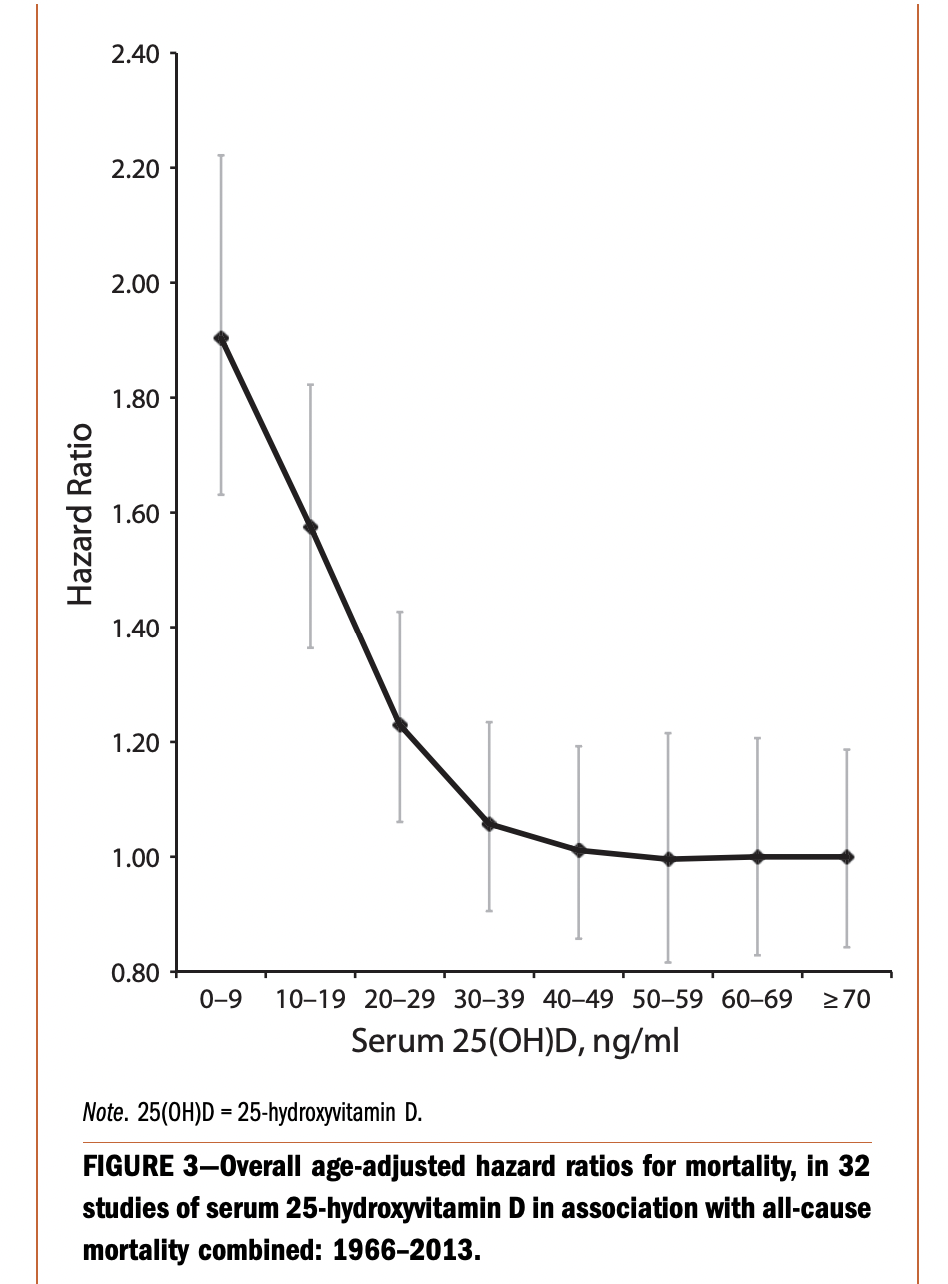
Here we can see that after 30 ng/ml (and maybe even after 25) differences arent significant (both statistically and practically).
This is just observational data which shows statistical relationship, but correlation isnt causation and its better to check interventional studies.
There some other studies which making recommendations to keep serum D3 levels >= 50 ng/ml. They are using the same approach - observational data analysis. They just look at serum D3 and found that the higher were levels were associated with the lower COVID mortality. This doesnt prove that supplementing until 50 ng/ml will give same results, because the ways people got D3 levels this high is unknown. For example, it might be due to a vacations in sunny places or getting a lot of sun through day. Getting active day on sun is not near the same as just taking D3 pills in the morning. For example, getting a sunny day on the beach will affect different things: lower stress levels, relax you, releases some nitric oxide which stabilise blood pressure which a things that improve overall health and wellbeing. We also can see novel evidence that sun expose improves sleep quality but D3 supplementation dont, but there are some that found opposite.
Anyway, we can see that supplementation for people with >= 20 ng/ml of serum vitamin D have little or no evidence of significant positive effects. There are more data from 2017 which show no improvement in ACM for people with >= 20 ng/ml when they supplement. Inverse ACM association was found only for group with deficit (< 20 ng/ml). According to that evidence vitamin D supplementation may be worthful only when serum levels are lower than 20 ng/ml.
Increased bone turnover, bone loss and bone mineralization issues happens in conditions when vitamin D < 20 ng/ml.
I conclude that supplementation during periods of serum vitamin D is less or near 20 ng/ml is worthful, but after it's increases over 30-35 ng/ml the evidence of significant improvements is weak. But some inspired fancy "sources" tells people to aim to 40-56 ng/ml or even more. From my perspective i dont see high quality scientific evidence for proving that choice.
Dosage & frequency
Before start interventions to increase D3 - serum levels must be measured by blood test. Firstly, we have to confirm that serum levels of active form of vitamin D3 - 25(OH)D is lower than ~25 ng/ml and in that case it might be worthful to take actions:
- Make sure foods with D3 is presented in diet
- Focus on non-supplemental interventions - get the sun exposure
- If it's not enough or not possible then it worth to look for D3 supplements.
From this study we can see that it's not an easy task to increase D3 levels by using sun (32% of participants didnt reach even 20 minutes per day), but people who achieved 30 mins were able to increase D3 by 4.5 ng/ml. Downside of this study is authors didnt reveal how much of skin area were exposed to sun. But we can see that 500 UI per day increased serum D3 by 8.5 ng/ml after 8 weeks of supplementation.
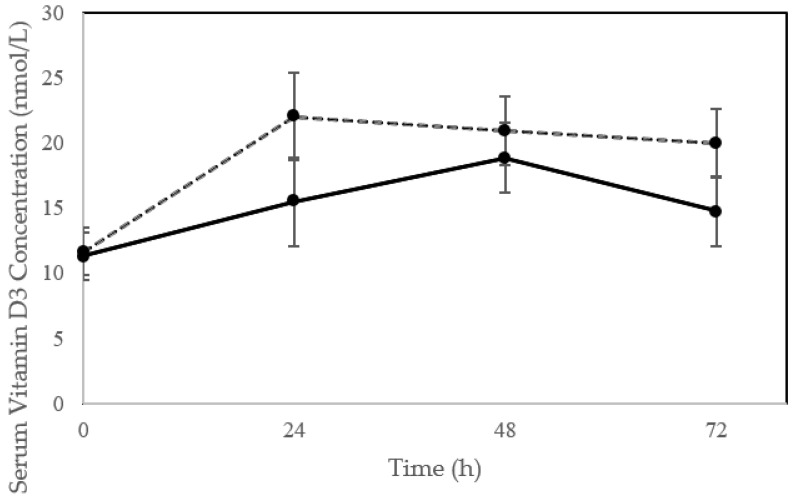
Getting sun exposure is preferable at the early morning or late evening to avoid skin sunburn which increase risk of skin cancer. The more skin surface exposed to sun the more D3 will be produced. This study aimed for 43% of skin exposure to sun and showed that single exposure significantly increased serum D3 levels. The black line for old people and dashed for young.
This data suggests that regular sun exposure of 40%+ of skin surface (remember than half of skin is not exposured) is enough to increase and maintain healthy D3 levels.
If sun exposure is not available then we might look for supplementation. Some publications about dosing and frequency provide evidence that using doses of 3000-4000 UI 4-5 day per week is enough to increase levels by +13 ng/ml, so if we at deficit <20ng/ml we would go up to 30+ ng/ml.
It is recommended to add vitamin K2 to D3 supplement routine (45-90 mg of K2 MK-7 should be enough). Since D3 is fat soluble, best absorption happens with meal containing some fat. Magnesium is required to activate D3, so just make sure there is enough leafy greens in diet (there is a lot of magnesium in chlorophyll).
Since each person will have specific D3 supplementation response, after 1-2 months of supplementation, taking a pause for 1-2 weeks and measuring 25(OH)D levels in blood allow to see the changes in D3 status. These change may lead us to updating strategy.
Timing
There are some limited data - 26 stories form Seth Roberts blog and his article (to view picture open as image in new tab and remove "blog." from url like that) that its better to take vitamin D in the morning, because taking it after may negatively affect sleep. Another part of evidence comes from Gwern Branwen. Scientists doesnt control for D3 timing, so can imagine priors as 50:50 for morning vs evening supplementation. Even despite evidence for morning is small, using Bayesian approach will adjust priors to favor the morning side.
P.S.
If you want to correct to me at some points, just leave a comment with sources to scientific studies.
The information presented here is for educational purposes and it's recommended to consult your physician before any interventions.